Insights from trauma therapy help us understand what goes on in our brain when we receive a cancer diagnosis.
Cancer diagnosis: nightmares, flashbacks, intrusions
- Cancer diagnosis: nightmares, flashbacks, intrusions
- Cancer diagnosis: how to cope with psychological stress
- Cancer diagnosis: guidelines for a discussion with treating doctors
- Basics
- Diagnostic
- Treatment
- Questions about current complaints / side effects
- Questions upon finishing medical treatment
- Questions in the event of a relapse
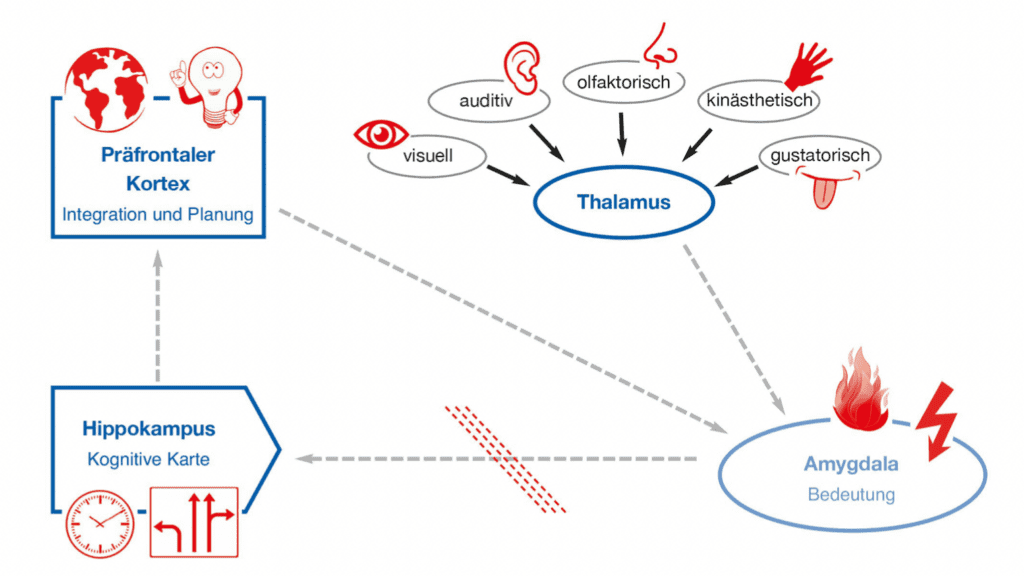
The “natural” pathways in the information processing system are blocked, which can lead to typical post-traumatic stress symptoms. Many people who have experienced a traumatic or highly frightening situation are familiar with some of these reactions: they are primarily sudden, overwhelming fears, images, and body feelings – switched on by some internal or external stimulus (trigger).
- For example, a patient regularly feels nauseous when she tries to have a red drink. She cannot explain this to herself. Eventually, it turns out that the infusion during her chemotherapy was red.
- Another patient always experiences intense fear and panic when trying to cross the street at certain traffic lights. It turns out that the traffic light made a particular crackling noise indicating the “green phase” for visually impaired people. This sound was similar to the sound of a device during her treatment that she had experienced as particularly distressing.
- Certain smells or body perceptions can also be triggers.
- For example, a patient reports that he can hardly concentrate on reading the daily newspaper or suddenly forgot the contents of the last few pages when reading a book.
- Another patient reports that she cannot remember what the doctor told her when she received the diagnosis. All she can remember is that he had a yellow and blue tie and looked worried. This shows that her amygdala was extremely overexcited, and the prefrontal cortex was “switched off”, especially its left, more rational regions, including the language centre.
Cancer diagnosis: how to cope with psychological stress
Nobody is “to blame” for your illness, not even you. Accept your disease like a stroke of fate. Take up the fight against your condition and find allies to support you. Become a supporter of your doctors in the battle against the disease. Discuss the treatment strategy with them and ask about anything unclear to you.
- Think of the people and things that have given you strength and hope in the past. Try to spend time with these people or things.
- If the treatment changes your appearance, remember: The most important thing about you is your inner being. The people who love you know this.
- Your illness requires time to heal, physically and mentally. Take plenty of time for yourself.
- Talk to other people about your feelings and fears. If you cannot or do not want to do this with relatives or friends, get in touch with those affected – for example, in self-help groups. Do not shut yourself away.
- Think positively about the future.
- When you cannot deal alone with your psychological stresses, seek the help of an experienced psycho-oncologist.
Another tip: deal openly with your illness and do not bottle up thoughts about it. Make sure, however, that your life is not all about it, but pursue your previous interests as much as possible.
Even if it sounds strange, many people affected report that their life became more intense due to the disease.
Cancer diagnosis: guidelines for a discussion with treating doctors
Talking to the treating doctor can often be stressful. Since great fear harms information processing, it helps to prepare such conversations. If possible, bring someone you trust with you to the interview. Four ears hear more than two.
Here you will find essential questions for discussions with a doctor and information on preparing for such a discussion. Depending on the treatment phase (diagnosis, treatment, follow-up care, etc.) you are in, you can pick the right questions for your doctor’s consultation.
Basics
- If you have any doubts about the procedure described or feel unsure, you can always obtain a second opinion.
- You also are entitled to get a second opinion from another pathologist if you are unsure whether the diagnosis is correct.
- You have a free choice of doctor.
- When important therapy decisions are pending, you should ask for a few days to think about it. That will not worsen your chances of recovery because immediate action is necessary for very few situations.
- If you must choose between different treatment options, you should do your research and take the time necessary to decide.
- Write down your questions in advance and write things down during the conversation to not forget anything during the conversation.
- Ask someone you trust to accompany you to the doctor’s appointment.
- Do not be afraid to ask if you did not understand something immediately, and ask several times – until you know it. Be brave and ask. Any question is allowed – as often as needed!
- Try to summarize the critical content of the conversation in your own words. That can avoid misunderstandings.
- Inform your doctor about critical disease-related aspects (e.g., current medications, including over-the-counter, naturopathic, or food supplements).
- Are there any other illnesses (e.g., diabetes, heart problems)?
- Ask the doctor to take some time, as everything is mostly new territory for you, while for the doctor, the topics and processes are more familiar.
- You have the right to view it in your medical record.
- Use the information from the pertaining patient guidelines – in Germany www.krebshilfe.de/informieren/ueberkrebs/infothek/infomaterialategorie/patientenleitlinien/
Diagnostic
- What is the exact diagnosis?
- How do you assess my situation?
- How far has cancer spread in my body?
- What stage is the disease, how advanced is it? How large is the tumour? Are the lymph nodes involved? Have metastases already formed?
- How will this disease affect my life, my work, my family? What changes should I expect?
- Should I actively make changes in my everyday life?
Treatment
- How is the further procedure? There are several treatment options ions?
- What treatment options are there and why?
- Which of the treatment options has the lowest risk of relapse?
- How much time will the therapies take? Will the treatment be inpatient or outpatient? How long will I be in the hospital, or will I be unable to work?
- How soon do I have to decide about the proposed treatment?
- How exactly does the treatment work, and to what extent?
- What is the name of the medication I will take? What are they for, and what do they do?
- How does the treatment affect the body and the course of the disease?
- What side effects do I have to expect?
- Are there differences in terms of long-term effects?
- What is the goal of the treatment? Is the disease curable in principle, or are we talking about an attempt to contain the disease and achieve the longest possible lifespan with a good quality of life? What is the difference between curative, adjuvant and palliative treatment?
- What are the options in case of relapse after the therapy or if metastases have formed?
- Is there any recent research or clinical study I should know?
- What happens after the treatment? Where can I get information about oncological rehabilitation and aftercare?
- Who can I contact if I have further questions?
- If you want to have children: will the treatment affect my fertility? If so, what are the options for maintaining fertility?
Questions about current complaints / side effects
- What ailments and symptoms do I currently have? How have these changed in the last few weeks/months?
- Can the treatment explain my complaints?
- What symptoms or problems should I discuss immediately at my doctor’s appointment?
- What possibilities of psychological / psycho-oncological support are there? Are there other support options (e.g., self-help groups)?
- Are there also support options for my family?
Questions upon finishing medical treatment
- How often do I have to have a follow-up examination?
- What will be other examinations necessary?
- If I have any symptoms, do I have to see a doctor immediately?
- How can I support my healing?
- What treatment options do I have if the cancer comes back?
- What psycho-oncological support options do I have if my fears increase and impair my quality of life? Where can I get psycho-oncological support? What other offers are there?
Questions in the event of a relapse
- In what form did the cancer return? Have metastases developed? Do I have a new tumour?
- What treatment options are there in my situation? Is a cure still possible?
- What side effects should I expect?
- What long-term consequences do I have to expect?
- Are there other treatment options if therapy does not work or if there is another relapse?
- Is it possible to be involved in a clinical study to obtain new drugs?
- How can I get psycho-oncological support to deal with this situation?
Sources:
Diegelmann, C., Isermann, M., Zimmermann, T.: Therapie-Tools Psychoonkologie. Beltz, Weinheim 2020.
Stiftung Deutsche Krebshilfe (Hrsg.): Die blauen Ratgeber. Brustkrebs. Antworten. Hilfen. Perspektiven. https://www.krebshilfe.de/informieren/ueber-krebs/infothek/
Mindfulness, Amygdala, Adjustment Disorder, Breast Cancer, Cancer, Limbic System, Psyche, Mental Health, Psychology, Psychotherapy, PTSD, Stress, Trauma